Abstract
Introduction
There are conflicting reports on the effects of angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) on acute pancreatitis incidence.
Objective
The aim was to determine whether use of ACE inhibitors and ARBs is associated with the incidence of acute pancreatitis, compared with use of dihydropyridine calcium channel blockers (dCCBs).
Methods
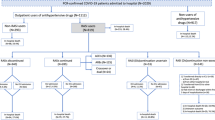
We assembled two population-based, new-user, active comparator cohorts using the United Kingdom Clinical Practice Research Datalink linked to the Hospital Episode Statistics repository and Office for National Statistics from 1998 to 2018, with follow-up until 2019. The first cohort included 304,083 ACE inhibitor initiators and 194,431 dCCB initiators. The second cohort included 29,160 ARB initiators and 203,610 dCCB initiators. Cox proportional hazards models were fit to estimate hazard ratios (HRs) with 95% confidence intervals (CIs) of acute pancreatitis, comparing ACE inhibitors and ARBs, separately, with dCCBs. Models were weighted using standardized mortality ratio weights generated from calendar time-specific propensity scores.
Results
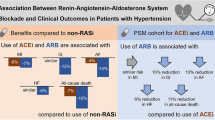
ACE inhibitors were associated with an increased risk of acute pancreatitis, compared with dCCBs (64.3 vs 45.2 per 100,000 person-years, respectively; HR 1.45, 95% CI 1.15–1.83). The number needed to harm after 2 and 5 years of use was 2438 and 1019, respectively. In contrast, ARBs were not associated with an increased risk of acute pancreatitis, compared with dCCBs (40.1 vs 47.6 per 100,000 person-years, respectively; HR 0.88, 95% CI 0.60–1.31).
Conclusions
ACE inhibitors were associated with a modest increased risk of acute pancreatitis compared with dCCBs. This association should be balanced with the known clinical benefits of ACE inhibitors in hypertension management. In contrast, no association was observed with ARBs.


Similar content being viewed by others
References
Williams B, et al. 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens. 2018;36(12):2284–309.
Whelton PK, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138(17):e426–83.
Hou FF, et al. Efficacy and safety of benazepril for advanced chronic renal insufficiency. N Engl J Med. 2006;354(2):131–40.
Kushner FG, et al. 2009 focused updates: ACC/AHA Guidelines for the management of patients with ST-Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120(22):2271–306.
Yancy CW, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136(6):e137–61.
Mederos MA, Reber HA, Girgis MD. Acute pancreatitis: a review. JAMA. 2021;325(4):382–90.
Peery AF, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology. 2019;156(1):254-272 e11.
Johnson CD, Besselink MG, Carter R. Acute pancreatitis. BMJ. 2014;349:g4859.
Fagenholz PJ, et al. Increasing United States hospital admissions for acute pancreatitis, 1988–2003. Ann Epidemiol. 2007;17(7):491–7.
Petrov MS, et al. Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis. Gastroenterology. 2010;139(3):813–20.
Zilio MB, et al. A systematic review and meta-analysis of the aetiology of acute pancreatitis. HPB (Oxford). 2019;21(3):259–67.
Forsmark CE, Vege SS, Wilcox CM. Acute Pancreatitis. N Engl J Med. 2016;375(20):1972–81.
Wolfe D, et al. Drug induced pancreatitis: A systematic review of case reports to determine potential drug associations. PLoS ONE. 2020;15(4):e0231883.
Lancashire RJ, Cheng K, Langman MJ. Discrepancies between population-based data and adverse reaction reports in assessing drugs as causes of acute pancreatitis. Aliment Pharmacol Ther. 2003;17(7):887–93.
Cheng RM, et al. Association between ACE inhibitors and acute pancreatitis in the elderly. Ann Pharmacother. 2003;37(7–8):994–8.
Eland IA, et al. Antihypertensive medication and the risk of acute pancreatitis: the European case-control study on drug-induced acute pancreatitis (EDIP). Scand J Gastroenterol. 2006;41(12):1484–90.
Douros A, et al. Drug-induced acute pancreatitis: results from the hospital-based Berlin case-control surveillance study of 102 cases. Aliment Pharmacol Ther. 2013;38(7):825–34.
Kuoppala J, et al. ACE inhibitors and the risk of acute pancreatitis-a population-based case-control study. Pharmacoepidemiol Drug Saf. 2017;26(7):853–7.
Bexelius TS, et al. Angiotensin II receptor blockers and risk of acute pancreatitis—a population based case-control study in Sweden. BMC Gastroenterol. 2017;17(1):36.
Sjoberg Bexelius T, Garcia Rodriguez LA, Lindblad M. Use of angiotensin II receptor blockers and the risk of acute pancreatitis: a nested case-control study. Pancreatology. 2009;9(6):786–92.
Lai SW, et al. No association between losartan use and acute pancreatitis in hypertensive patients. Eur J Hosp Pharm. 2017;24(2):120–3.
Bas M, et al. Nonallergic angioedema: role of bradykinin. Allergy. 2007;62(8):842–56.
Hirata M, et al. Blockade of bradykinin B(2) receptor suppresses acute pancreatitis induced by obstruction of the pancreaticobiliary duct in rats. Br J Pharmacol. 2002;135(1):29–36.
Bhaskaran K, et al. Representativeness and optimal use of body mass index (BMI) in the UK Clinical Practice Research Datalink (CPRD). BMJ Open. 2013;3(9):e003389.
Mathur R, et al. Completeness and usability of ethnicity data in UK-based primary care and hospital databases. J Public Health (Oxf). 2014;36(4):684–92.
Herrett E, et al. Data resource profile: clinical practice research datalink (CPRD). Int J Epidemiol. 2015;44(3):827–36.
Herrett E, et al. Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol. 2010;69(1):4–14.
Herbert A, et al. Data resource profile: hospital episode statistics admitted patient care (HES APC). Int J Epidemiol. 2017;46(4):1093–1093i.
Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8(5):551–61.
Mack CD, et al. Calendar time-specific propensity scores and comparative effectiveness research for stage III colon cancer chemotherapy. Pharmacoepidemiol Drug Saf. 2013;22(8):810–8.
Sato T, Matsuyama Y. Marginal structural models as a tool for standardization. Epidemiology. 2003;14(6):680–6.
Suissa D, et al. Number needed to treat is incorrect without proper time-related considerations. J Clin Epidemiol. 2012;65(1):42–6.
Tilkemeier P, Thompson PD. Acute pancreatitis possibly related to enalapril. N Engl J Med. 1988;318(19):1275–6.
Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158(9):915–20.
Wei J, et al. Comparison of cardiovascular events among users of different classes of antihypertension medications: a systematic review and network meta-analysis. JAMA Netw Open. 2020;3(2):e1921618.
Santos D, Dhamoon MS. Trends in antihypertensive medication use among individuals with a history of stroke and hypertension, 2005 to 2016. JAMA Neurol. 2020;77(11):1382–9.
Derington CG, et al. Trends in antihypertensive medication monotherapy and combination use among US adults, national health and nutrition examination survey 2005–2016. Hypertension. 2020;75(4):973–81.
Kaurich T. Drug-induced acute pancreatitis. Proc (Bayl Univ Med Cent). 2008;21(1):77–81.
Griesbacher T. Kallikrein-kinin system in acute pancreatitis: potential of B(2)-bradykinin antagonists and kallikrein inhibitors. Pharmacology. 2000;60(3):113–20.
Hussain MS, et al. Angiotensin-Converting Enzyme (ACE) Inhibitors and Pancreatitis: A Potential Dose-dependent Relationship. Eur J Case Rep Intern Med. 2020;7(12):001956.
Jones MR, et al. Drug-induced acute pancreatitis: a review. Ochsner J. 2015;15(1):45–51.
Yamada T, et al. Candesartan, an angiotensin II receptor antagonist, suppresses pancreatic inflammation and fibrosis in rats. J Pharmacol Exp Ther. 2003;307(1):17–23.
Boffa RJ, et al. Hypertension in adults: summary of updated NICE guidance. BMJ. 2019;367:l5310.
Mejzner N, et al. Trends in the diagnosis and management of hypertension: repeated primary care survey in South West England. Br J Gen Pract. 2017;67(658):e306–13.
Mansfield K, et al. Completeness and validity of alcohol recording in general practice within the UK: a cross-sectional study. BMJ Open. 2019;9(11):e031537.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by a Foundation Scheme grant from the Canadian Institutes of Health Research (FDN-143328). JR is the recipient of a Doctoral Award from the Canadian Institutes of Health Research (FRN-152254) and a Doctoral Award from the Fonds de Recherche du Québec- Santé. EGM holds a Chercheur-Clinicien Junior 1 award from the Fonds de Recherche du Québec- Santé. LA holds a Chercheur-Boursier Senior Award from the Fonds de Recherche du Québec - Santé and is the recipient of a William Dawson Scholar award from McGill University. The funding sources had no influence on the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflict of interest
JR received consulting fees for work unrelated to this study from Biogen. LA received consulting fees from Janssen and Pfizer for work unrelated to this study. HY, EGM, and AB have no conflicts to disclose.
Ethical approval
The study complied with the Declaration of Helsinki. The study protocol was approved by the Independent Scientific Advisory Committee of the CPRD (protocol number 20_000225R) and the Research Ethics Board of the Jewish General Hospital, Montreal, Canada (number 2021-2748).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Author contribution
All authors conceived and designed the study, interpreted the data, critically revised the manuscript for important intellectual content, and approved the final version of the manuscript. LA acquired the data. JR, HY, and LA conducted the analyses. JR drafted the manuscript. LA attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. LA is accountable for all aspects of the work.
Data and code availability
The data cannot be shared publicly due to the privacy policy of the Clinical Practice Research Datalink.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rouette, J., Yin, H., McDonald, E.G. et al. Renin–Angiotensin–Aldosterone System Inhibitors and Risk of Acute Pancreatitis: A Population-Based Cohort Study. Drug Saf 45, 65–74 (2022). https://doi.org/10.1007/s40264-021-01128-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-021-01128-1