Expert Advice #4
Children, Covid-19 and Classrooms: A 10-point Plan for Making Schooling Safe

This is the fourth of a series of expert advisories on how to respond to Covid-19 published from time to time by Maverick Citizen.
The previous advisories were:
- How long should I isolate or quarantine for? (here)
- Practical guidance on disinfecting (here)
- Testing for Covid-19? All you need to know about antibody tests (here)
The series is co-written by some of South Africa’s leading medical scientists and academics, including some members of the Ministerial Advisory Committee (MAC) on Covid-19. It is intended to provide practical life-saving advice based on the best emerging knowledge and evidence of Covid-19.
We are learning all the time, so it is highly likely that advice will change as we learn more about the virus, so keep an eye on any new recommendations. However, the basic principles explained in this series will stand and help inform your decisions.
Back to school: What’s at stake?
The return of children to school both in South Africa and globally has introduced anxiety at many levels within society. Parents are concerned that their children may become infected with Covid-19 while at school, teachers fear for their own health and many families worry that the school-going child will bring Covid-19 into the household.
With the easing of lockdown restrictions and with parents returning to work, there is a growing need for reassurance that school-going children will be safe. Teachers too need support in reducing risk in their classrooms and minimising school-based transmission.
To ease anxiety, let’s start with what we know about Covid-19 in children:
Paediatric associations, paediatricians, public health specialists and educationists have all encouraged the opening of schools, arguing that the risk-benefit ratio tilts favourably towards the resumption of face-to-face teaching.
Both the South African Paediatric Association (SAPA) and the South African Medical Association (SAMA) are supportive of the return to school and their recommendations align with several scientific findings including:
- Lower risk of Covid-19 acquisition in children compared with adults;
- Very low risk of Covid-19-related death in children;
- Likely lower transmission risk from children to adults;
- Low risk of children contributing to outbreaks in school;
- Low prevalence of comorbidities (diseases like hypertension, diabetes) in children; and
- Increased collateral damage and adverse effects of school closure on child nutrition, learning, cognitive development and mental health especially for children in lower socio-economic households and communities.
This stance is supported by other international paediatric associations such as the American Academy of Pediatrics (AAP) and the United Kingdom’s Royal College of Paediatrics and Child Health. The AAP says children learn best when they are at school.
Statistics on Covid-19 in children in South Africa
Currently, children and adolescents of 18 and younger constitute just over one third (35.1%; 20,633,557) of the population, yet only 7% (33065/445432) of all reported Covid-19 cases have occurred in this age group.
As reflected in Figure 1 (below), the number of cases in young people is far smaller than in older population groups and this trend is particularly pronounced in children less than 10 years old
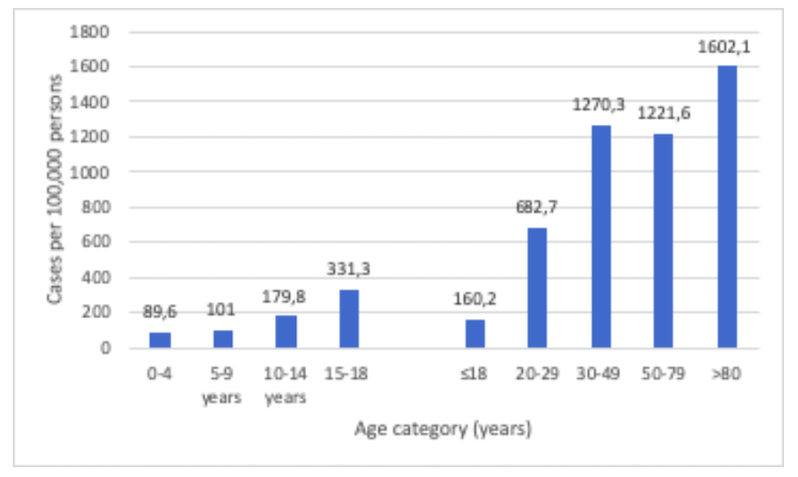
Figure 1: Differences in Covid-19 cases in younger versus older age groups in South Africa. Source: Source: National Institute of Communicable Diseases (NICD), National Health Laboratory Services (NHLS), August 2020
From the NICD’s hospital surveillance in South Africa, only 3.2% (1,067 out 33,318) hospitalisations were in children under 18 years of age.
Of all the deaths in South Africa, to date, less than 1% occurred in children. Indeed, like all countries in the world, death from Covid-19 is a rare event in childhood.
Attending school is essential for other aspects of children’s health and development
The extended period of school closures (March 2020-June/July 2020, depending on grade, and again during July-August 2020) has had immense ramifications on childrens’ nutrition, learning, cognitive development, socialisation and mental health.
For example, our National School Nutrition Programme (NSNP) provides daily meals to approximately 9.6 million learners nationwide in 20,619 schools. The provision of meals has additional spin-offs including increased levels of attendance, concentration, as well as retention in school.
The NIDS-CRAM survey reported that since the start of lockdown one in seven people surveyed reported that a child had gone hungry in their household in the past week. Additionally, six million of our 20 million children live in households with no employed adults, and approximately one third (6.4 million children) live in households where family income is below the food poverty line.
Consequently, the NSNP plays a critical role for our children, so much so that school closure has amplified extreme hunger in children. Although the recent court ruling in the Pretoria High Court de-links the provision of food from schools being opened or closed for teaching, there has been tremendous difficulty in executing this function during the pandemic and even after the court order many children are still going without food as schooling remains disrupted.
Do children infect teachers with Covid-19?
By 5 July 2020, the Department of Basic Education (DBE) has documented that 2,740 out of 440,000 teachers and 1,260 learners have been infected, representing 0.62% of teachers, and 0.01% of learners. This is in line with the national infection trends.
Current data suggests that the risk among younger school children spreading the virus to teachers has been low. Research has shown that children under 10 years are probably less effective transmitters of Covid-19 and infrequently serve as the index (first) case in Covid-19 family clusters or in community spread. Children and young people (under 20 years) have a lower susceptibility to Covid-19, with 56% lower odds than adults of being an infected contact of someone who tests positive for Covid-19.
As children get older and bigger, they are more capable of transmitting Covid-19, so it is very important to introduce measures in schools such as physical distancing, handwashing and wearing masks to reduce transmission, and to reinforce these measures among teenage school-goers.
***
A 10-point Plan for keeping schools safe
The 10-point Plan we suggest below is based on the best knowledge available to us and is consistent with the DBE’s guidance on keeping schools safe when re-opening.
Remember: Well ventilated school environments that minimise congestion and crowding should be the overall goal of every school.
- Set up a Covid-19 School Management Team led by the school principal and designate a staff member who is the Covid-19 point of contact at the school with whom parents and students can communicate. Know who the local (district) public health official is in case you need advice. Alternatively, the NICD/NDOH hotline (0800 029 999) will serve as a useful resource.
- Implement non-pharmaceutical interventions: physical distancing, regular hand washing or use of hand sanitisers, practising cough etiquette and the wearing of masks for everyone. Reinforce these throughout the day and especially among teenage school-goers. If learners are unable to afford a mask, a T-shirt, scarf or buff will serve as an adequate and appropriate facial barrier.
- Know the age profile and comorbidities of your teachers. Teachers who are older than 60, who have diabetes, hypertension, obesity are at higher risk of adverse illness. These teachers can be asked to play a supportive role in teaching (teaching preparation, supporting online/remote teaching, marking, administration), as per the DBE regulations.
- Know which children are sick or who have a relevant comorbidity that places them at risk of severe Covid-19. Have a plan for them to be supported with remote learning should the need arise.
- Limit the use of the tea room for teachers and limit in-person meetings with other adults to a maximum of five. Ensure that there is always adequate space for 1.5m physical distancing if meetings must be held indoors. Inside meetings should occur in well-ventilated rooms with windows open.
- Make sure the classrooms, desks and surfaces are cleaned twice every day as per DBE requirements.
- For lower grades children could remain in the classroom and teachers could move from class to class as this may limit crowding and congestion; this may not be feasible for higher grades given subject choices. For all grades consider implementing alternate-day face to face teaching with half classes consider implementing alternate-day face to face teaching with half classes; or have one set of classes in the morning and the other set in the afternoon. Holding classes in shifts, as per DBE regulations and time-tabling guidelines reduces the class size. In considering having desks 1m apart, the use of desk shields/partitions or face masks would more than suffice to address the physical distancing. The physical distancing is especially important when there is no other barriers in place between people.
- Implement physical distancing in the classroom: desks to be spaced 1.5m apart. Discourage sharing food, containers and utensils.
- Use outdoor spaces as much as possible.
- Conduct daily checks with your staff and learners as per the DBE/DOH Screening Guidelines: symptom check and temperature evaluation may have a supportive role. The DBE Standard Operating procedures provide guidance in this regard.
***
FREQUENTLY ASKED QUESTIONS
***
If a learner tests positive, who is a ‘contact’ and who must quarantine?
Identification of close contacts follows national guidelines. Current guidance divides contacts into close and casual.
If desks are spaced at more than 1.5 m, ventilation has been adequate, and all learners have been wearing masks then the learners in the class are considered casual contacts and do not have to quarantine.
However, if there are concerns that distancing was not maintained, and/or masks not worn correctly and/or ventilation was poor, then the learners in the class sitting circumferentially closest to the learner who tested positive (that is surrounding the learner on all sides), are considered close contacts and should quarantine as per the current Department of Health protocols.
The decision on who is a close and who is a casual contact should ideally be made in consultation with the local public health official if the school feels uncertain. Where there is difficulty in accessing adequate health advice we recommend contacting the NICD/NDOH hotline (0800 029 999).
***
What should schools do if a learner (or member of their family) or teacher or staff member tests positive or appears to be symptomatic for Covid-19 while at school?
Each school should have a clear plan and protocol to follow if someone develops symptoms at school. As recommended in the 10-Point Plan above, a designated staff member who is responsible for managing the protocol should be identified in advance. Regular communication with the school community should be a key part of the management plan.
First and foremost, each school must identify a room or a space to locate someone who is symptomatic until they are able to go home.
Any learner or teacher who tests positive should not go to school under any circumstance.
For children in boarding school, a Covid-19 positive child should be moved to a place that minimises contacts with peers (a designated sick room, or open area that limits access to other students or staff members).
The overall aim here is to reduce the risk of transmission.
In this area, there should be good ventilation, hand sanitisers/soap and water. If the space is a room, it should have windows that can be opened, a door that can shut, a plastic chair or a chair that can be easily cleaned, a table with hand sanitiser, tissues and disinfectants to clean surfaces and a bin that has a plastic bag for waste. The room should not have a carpet. Having a basin with running water in the room is an advantage, but not mandatory. Make sure there is a supply of masks in the room. If there is no room available, look after the individual on a chair in an open area.
If a learner/teacher develops symptoms in school, the designated staff member should be alerted to manage the process. At all times show compassion for the individual to avoid stigma among the school community and accompany the individual calmly to the demarcated area.
Do not allow friends or others to sit with the individual. Allow 2m between any other people in the vicinity. Confirm that there is good ventilation in the area.
Ensure that the individual’s mask is covering the nose and mouth adequately. Ask the individual to thoroughly wash their hands for 20 seconds. If tissues are used, the individual should put the tissues used into the plastic bag in the bin. If there are no tissues, ask the individual to sneeze or cough into the crook of their elbow. If they need to go to the bathroom, a separate toilet should be used. When flushing the toilet, the lid of the toilet must be closed. Wash hands for 20 seconds after going to the toilet.
Once the individual has been transferred out of the school, this area and the classroom should be thoroughly cleaned. The chair or desk should be wiped down. The cleaning of the room should take place with staff using surgical masks, gloves and plastic aprons. All materials must be disposed of in the plastic bag in the bin. The plastic bag must be sealed and disposed of in an outside bin.
Only close contacts should quarantine as per national guidelines.
The principal should communicate weekly with the school community outlining the number of individuals isolating and in quarantine to avoid unnecessary rumour and panic.
We do not recommend school closure or class closure. We recommend isolating the Covid-19 positive individual (learner/teacher/admin/support staff) and quarantining close contacts. Learners and teachers who are not close contacts can continue going to school while conducting daily symptom screening for 14 days.
Community transmission and cases in schools will occur. This does not necessitate anything more than isolating the case and quarantining close contacts. If this advice is followed, we will prevent the loss of much-needed teaching time.
***
I am a teacher with comorbidities — should I be teaching?
If you are a teacher who is over 60 and you have comorbidities such as obesity, hypertension, diabetes, chronic heart or kidney disease, cancer, HIV or TB, you should consult your clinic or your doctor before going back to school.
Your doctor or clinic will evaluate your health and assess how well your chronic illness is controlled and give you advice about whether you should be teaching. DBE procedures will need to be applied for absence from teaching.
It may be preferable for you not to do face-to-face teaching, and rather support your colleagues by doing online teaching, where feasible, or helping them prepare their lessons, marking, setting tests and exams etc, as directed by the principal.
While you are at school, remember not to be in close contact with your fellow teachers, keep at least 1.5m from other adults and avoid congregating in tea rooms or at staff meetings. Keep wearing your mask, use a visor (costed from R20), keep your nose covered, keep washing your hands and keep the surfaces near you clean. Keep the area where you work well ventilated. Avoid crowds and congestion. Keep taking your medications and practice physical distancing wherever you are, especially in your community.
Remember your biggest risk for getting Covid-19 will be at home in the community. Your first step is to ensure that in your daily life you are taking steps to minimise your risks for getting Covid-19, by practicing physical distancing, wearing masks and washing your hands regularly. You should avoid congested areas, crowds and also make sure there is good ventilation in the areas you are frequenting.
***
I have an elderly grandparent or family member at home — should I send my child to school?
If you have elderly members of your family living with you there are certain practices you may need to entrench at home. If you have toddlers or small children that are going to daycare, pre-school or nursery school you may want to minimise prolonged physical contact with elderly grandparents/uncles and aunts. The overall objective is to try to lower the risk in your home as much as possible.
The same basic rules apply:
- Maintain physical distance as much as possible.
- Never be in close contact with an elderly member of the family for more than 15 minutes.
- Always make sure that everyone keeps their masks on in their presence. Using face shields may be a good idea in the home.
- Wash your hands with soap and water regularly throughout the day.
- Keep your home well ventilated and windows open.
- Encourage your elderly relatives to keep 1.5-2m from everyone else in the household.
- Keep surfaces clean with disinfectants.
- Keep an eye out for symptoms of Covid-19 among family members. If there is a close contact, suggest quarantine for the elderly family member in a designated government quarantine facility.
- Make sure you understand risk factors for your family getting Covid-19 and try to minimise them e.g. don’t use public transport in peak periods where taxis are congested. Keep windows in taxis open, use a face shield and a mask. Keep sanitising your hands. Avoid crowds and congested places.
- Ensure household members cough or sneeze into the crook of their elbows, and dispose of tissues into plastic bags that are disposed of in an outside bin.
***
My child has a comorbidity (for example, congenital heart disease, cancer, kidney disease, cardiovascular disease, diabetes) — should I send him/her back to school?
First of all contact a clinic or doctor if you think your child has a comorbidity, or speak to the school. We understand that parents will be anxious about the health of their children. However, you need to try to keep your child in the school system. Being absent from school represents a loss of learning time.
As healthcare workers with experience in paediatrics, infectious diseases and public health, we recommend that children and adolescents with comorbidities should not be treated any differently from other children in terms of going back to school.
If you are concerned about your child’s health, consult a doctor or your clinic for advice about schooling. Remember if children take their medication regularly and are generally in good health, they should be able to go to school.
It is important to let the school know if your child has an illness. This will help them be supported at school. If children become ill, they or their caregivers should not delay in contacting their healthcare provider. Remember unmanaged illness is far more dangerous to a child’s health than the fear of Covid-19.
Factors to consider when deciding not to send your child to school include your ability to home-school, your access to remote-schooling and issues of home supervision. The DBE has procedures to be followed when a family chooses to not send a child to school because of a medical condition, family anxiety or preference. School will be able to guide families through the application procedure and will arrange for learning material to be collected by the family.
Always make sure your child is aware of their illness. Get them used to wearing masks, sanitising or washing their hands regularly and keeping away from crowds.
***
What about sporting activities and choirs?
We don’t recommend any activities that involve singing and choirs, even in open areas.
For sport, we recommend not sharing equipment or gear. Ensure that equipment is disinfected and ensure minimal use of communal areas such as locker area/ablutions.
Be aware of levels of risk:
- Lowest risk: Performing skill-building drills or conditioning at home, alone or with family members.
- Increasing risk: Team-based practice.
- More risk: Within-team competition.
- Even more risk: Full competition between teams from the same local geographic area.
- Highest risk: Full competition between teams from different geographic areas.
Risk is assessed based on:
- Physical closeness of players during play (closer = higher risk);
- Amount of necessary touching of shared equipment and gear (more touch = higher risk);
- Ability to engage in physical distancing while not actively engaged in play such as when on the bench or on the side-line;
- Age of the player and their ability to comply with physical distancing and other protective actions;
- Size of the team and field of play (more players and small field = higher risk);
- Presence of nonessential visitors, spectators, volunteers during practices or games (avoid non-essential visitors/spectators);
- Travel required outside of the local community (minimise travel).
The Centers for Disease Control and Prevention (CDC) in the US has guidance or recommendations on sport (here and here) that can be adapted by schools in South Africa.
***
Conclusion
In summary, school attendance has nutritional, educational, cognitive, social and mental health benefits. Learners are not at the highest risk of infection or death from Covid-19, and all decisions should be based on emerging data, some of which we have presented above.
Schools should be opened and should remain open while facilitating non-pharmaceutical measures in the school environment and among learners and teachers. Children/teachers with individual needs should consult a health worker to assess their risk, and an individualised plan should be devised accordingly. DM/MC
Selected References:
- Department of Basic Education Guidelines and Explaining Covid-19 to Kids here.
- Viner et al: Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: a systematic review and meta-analysis, available here.
- UNICEF, Covid-19 and Children, available here.
Authors:
This advisory has been compiled by a collective of educationists, paediatricians and infectious disease specialists including:
Professor Glenda Gray, President & CEO SAMRC, Research Professor in Paediatrics, Faculty of Health Sciences, University of Witwatersrand;
Dr Waasila Jassat, National Institute of Communicable Diseases, National Health Laboratory Services;
Professor Refiloe Masekela, Department of Paediatrics and Child Health, Nelson R Mandela School of Clinical Medicine, College of Health Science, UKZN;
Trisha Ramraj, Health Systems Research Unit, SAMRC.
Professor Shabir Madhi, Professor of Vaccinology: University of Witwatersrand. Director: SAMRC Vaccines and Infectious Diseases Analytics Research Unit (VIDA); DST/NRF South African Research Chair: Vaccine Preventable Diseases; Co-Director African Leadership in Vaccinology Expertise (ALIVE);
Dr Nandi Siegfried, Health Systems Research Unit, SAMRC, and University of Cape Town;
Professor Lucille Blumberg, National Institute for Communicable Disease, National Health Laboratory Services;
Professor Ameena Goga; Interim Director HIV Prevention Research Unit, SAMRC, and University of Pretoria;
Professor Robin Green, Chairman School of Medicine, University of Pretoria;
Dr Jeremy Nel, Helen Joseph Hospital, University of Witwatersrand;
Marilyn Stern, Educator;
Professor Francois Venter, Ezintsha, Faculty of Health Sciences, University of Witwatersrand;
Dr Matthew Chersich, WRHI, Faculty of Health Sciences, University of Witwatersrand;
Dr Aslam Dasoo. Progressive Health Forum;
Dr Faith Kumalo, Department of Basic Education;
Mary Metcalfe, PILO, and Senior Research Associate, University of Johannesburg.
"Information pertaining to Covid-19, vaccines, how to control the spread of the virus and potential treatments is ever-changing. Under the South African Disaster Management Act Regulation 11(5)(c) it is prohibited to publish information through any medium with the intention to deceive people on government measures to address COVID-19. We are therefore disabling the comment section on this article in order to protect both the commenting member and ourselves from potential liability. Should you have additional information that you think we should know, please email [email protected]"



 Become an Insider
Become an Insider