Most of the assessment tools used in our country examine a limited range of suicidal behaviours. In contrast, the Self-Injurious Thoughts and Behaviours Interview (SITBI), developed in the US, assesses a wider range of these behaviours: suicidal ideation, suicide attempt, suicidal gestures, and self-harming behaviours. Given this lack, we think it is necessary to validate the Escala de pensamientos and conductas autolesivas (EPCA), Spanish translation of the SITBI, in the Spanish population.
Material and methodsThe EPCA interview was administered to 150 inpatients in the Psychiatry Unit-Fundación Jiménez Díaz in order to examine its psychometric properties in a Spanish sample. To assess its test–retest reliability, the EPCA was again administered to those patients who were readmitted to hospital at least 6 months after the first assessment (n=50). To examine its construct validity, some of the most used assessment tools in this research field were also administered.
ResultsInter-rater agreement ranged from k=.90 to k=1. Test–retest reliability was good in the case of suicidal ideation, suicide plans and suicide attempts; however, it was lower in the case of self-harming behaviours and suicidal gestures. Our results also support the construct validity of the scale.
ConclusionsOur findings back the reliability (both inter-rater and test–retest) and construct validity of the EPCA in the Spanish population.
La mayor parte de instrumentos de evaluación que se utilizan en nuestro país examinan un rango limitado de conductas suicidas. En cambio, la escala Self-Injurious Thoughts and Behaviours Interview (SITBI), desarrollada en EE. UU., valora un rango más amplio de dichas conductas: intento de suicidio, ideación suicida, gestos suicidas y conductas autolesivas. Dada la carencia señalada, nos parece necesario validar la escala de pensamientos y conductas autolesivas (EPCA), traducción de la escala SITBI, en la población española.
Material y métodosCon objeto de examinar las propiedades psicométricas de la EPCA en una muestra española, la escala se administró a 150 adultos hospitalizados en el Servicio de Psiquiatría de la Fundación Jiménez Díaz. Para evaluar la fiabilidad test-retest de la escala, el protocolo de evaluación se volvió a administrar a todos aquellos pacientes que volvieron a ingresar en nuestra unidad al menos 6 meses después de la primera evaluación (n=50). Para valorar la validez de constructo de nuestra escala, se administraron algunas de las escalas de evaluación de suicidio más utilizadas en nuestro país.
ResultadosEl acuerdo entre examinadores osciló entre k = 0,90 y 1. La fiabilidad test-retest fue muy buena en el caso de la ideación suicida, los planes suicidas y los intentos de suicidio; no obstante, fue inferior en el caso de las autolesiones y los gestos suicidas. Nuestros resultados apoyan también la validez de constructo de nuestra escala.
ConclusionesNuestros resultados apoyan la fiabilidad (tanto entre-examinadores como test-retest) y validez de constructo de la EPCA en población española.
Despite the fact that great advances have been made in the study of suicidal behaviours in the last few decades, the measurements of suicidal behaviours used in both research as well as in clinical settings lack clarity and consistency.1 An important limitation of almost all the existing instruments (even those that include clear, specific definitions of the various suicidal behaviours) is that they examine only a limited range of such behaviours. In particular, the majority assess suicidal ideation; a lesser number of instruments assess suicide attempts; and a minority evaluate suicide planning, gestures or self-harm. This fact limits the availability of information on less studied constructs: suicidal gestures and self-harm.2 It also makes comparing different studies more difficult and preventing examining the relationships among the different types of suicidal behaviour.1 This last aspect is very important, as it can help clinicians to understand when and how these behaviours are related, especially bearing in mind that the less serious types of suicidal behaviour are the best predictors of the most serious suicidal behaviours.1 Specifically, the presences of a suicide plan and of self-harm are related with a greater risk of suicide attempt.3,4
The Self-Injurious Thoughts and Behaviours Interview (SITBI), developed in the Department of Psychiatry of the University of Harvard by Nock et al.,1 is the ideal complement to other measures of suicidal behaviour. The reason why is that, in addition to evaluating self-harm behaviours, it makes it possible to assess suicidal gestures and differentiate them from suicide attempts themselves.
The SITBI assesses the following aspects of each type of suicidal behaviour (suicidal ideation, suicide plans, suicide attempts, suicidal gestures and self-injurious behaviours): age at onset, method, severity, function, triggers, pain felt, associated consumption of alcohol or drugs, impulsiveness and influence of the environment.
At present, the short protocol of suicide assessment developed by various research groups in our country together5 is the only instrument that evaluates the entire range of suicidal behaviours, except for self-injurious behaviours. We also lack an instrument to discriminate between suicide attempts and suicidal gestures. For that reason, we felt that it was necessary to validate the translation of the SITBI scale into Spanish, the Escala de pensamientos and conductas autolesivas (EPCA), in the Spanish population. The SITBI has already demonstrated its usefulness in other countries such as the United States.6,7
This article presents the EPCA scale and preliminary results on its psychometric characteristics, including descriptive statistics, inter-rater reliability for the quantitative items, test–retest reliability for the items that examine the presence and frequency of each type of self-injurious behaviour in a period of 6 months and construct validity in relation to other scales used in this research area.
Material and methodsParticipantsTo examine the psychometric properties of the EPCA scale in a Spanish sample, the scale was given to 150 adult patients hospitalised in the Psychiatric Service of the Fundación Jiménez Díaz (Madrid) that had made a suicide or parasuicide attempt, presented self-injurious ideation and/or had carried out self-destructive behaviour without suicidal intention according to the definitions established in this research area.8 The patients were included in the study after signing an informed consent validated by the Ethics Committee to participate in this research. The recruitment period was between 1 December 2010 and 31 August 2011. A total of 6 patients rejected participating in the study. Patients that lacked the capacity to understand the study questions due to cognitive deterioration or mental retardation were excluded from the study. Based on those criteria, we excluded 2 subjects.
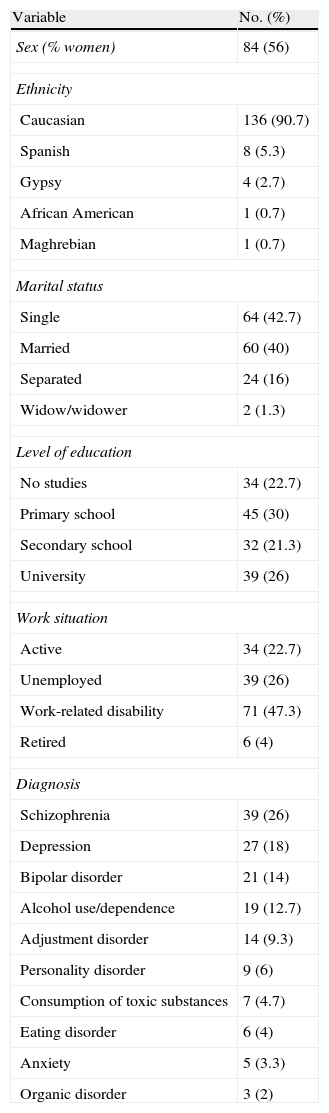
Most participants were women, Caucasian and single. The mean participant age was 43.3 years (SD=10.3). In Table 1, more detailed information on the demographic and diagnostic characteristics of the participants is presented.
Sociodemographic and diagnostic characteristics of the participants.
| Variable | No. (%) |
| Sex (% women) | 84 (56) |
| Ethnicity | |
| Caucasian | 136 (90.7) |
| Spanish | 8 (5.3) |
| Gypsy | 4 (2.7) |
| African American | 1 (0.7) |
| Maghrebian | 1 (0.7) |
| Marital status | |
| Single | 64 (42.7) |
| Married | 60 (40) |
| Separated | 24 (16) |
| Widow/widower | 2 (1.3) |
| Level of education | |
| No studies | 34 (22.7) |
| Primary school | 45 (30) |
| Secondary school | 32 (21.3) |
| University | 39 (26) |
| Work situation | |
| Active | 34 (22.7) |
| Unemployed | 39 (26) |
| Work-related disability | 71 (47.3) |
| Retired | 6 (4) |
| Diagnosis | |
| Schizophrenia | 39 (26) |
| Depression | 27 (18) |
| Bipolar disorder | 21 (14) |
| Alcohol use/dependence | 19 (12.7) |
| Adjustment disorder | 14 (9.3) |
| Personality disorder | 9 (6) |
| Consumption of toxic substances | 7 (4.7) |
| Eating disorder | 6 (4) |
| Anxiety | 5 (3.3) |
| Organic disorder | 3 (2) |
The process of translating the scale involved a inverse translation design, to ensure maximum equivalence of the 2 versions. In this translation, 2 bilingual mental health specialists participated (R. G. N. N. W.). The discrepancies between both translations were resolved by consensus. The EPCA scale is presented in the Appendix (available online as additional material).
Before beginning the process of sample collection, a clinical psychologist (R. G. N.), expert in administering tests, trained 2 psychiatrists and 2 psychologists to ensure that administration conditions were the same. The training phase ended when 100% agreement was reached in correcting and scoring the scale. The participants were randomly assigned to the interviewers.
AssessmentWe administered all participants the EPCA scale, a structured interview that consisted of 169 items divided into 5 modules that examined the presence, frequency and characteristics of 5 types of self-injurious behaviours: (a) suicidal ideation; (b) suicide plans; (c) suicidal gestures; (d) suicide attempts and (e) self-injuries. The construction of the questions in the original SITBI are consistent with the commonly accepted definitions of each type of behaviour.8,9
Each module begins with a screening question about the presence of lifetime self-injurious thought or behaviour. If the participant denies ever having presented such behaviour, a skip is made to the following module. If the participant states that such conduct has been presented, all the information relating to the following factors is sought: the frequency of self-injurious behaviour during each patient's lifetime, during the past year and the past month; the age at onset; the severity and the methods used. Next, the EPCA scale evaluates the function that each type of behaviour fulfils for the patient, by means of 4 questions whose responses are scored on a Likert scale from 0 to 4. The functions assessed are: emotional regulation (e.g., to avoid adverse feelings or generating feelings) or a means of communication with others (e.g., to attract the attention of others or to escape from some situation).
The EPCA also examines triggers, pain experienced and the influence of the environment in the self-injurious behaviour: the family, friends, partner, work mates, work/study and mental state. The participants are also asked about alcohol/drug use at the moment of self-injurious behaviour and its degree of premeditation or impulsiveness.
It takes from 3 to 15min to administer the scale, depending on the number of modules administered. In addition to the EPCA, to evaluate the construct validity of our scale, other related scales were administered: the Beck scale for suicide ideation (BSS),10 Beck suicidal intent scale (SIS),11 lethality rating scale (LRS)12 and the risk-rescue scale (RRS).13 All these scales are widely used in this research area and have generally shown good psychometric properties. Besides the previous scales, the following diagnostic instruments were administered: the mini-international neuropsychiatric interview (MINI)14 and the international personality disorder examination screening questionnaire (IPDE-SQ).15
To assess the test–retest reliability of the scale, the assessment protocol was again administered to all the patients that were admitted to our unit again at 6 months after the first assessment (n=50). We chose to examine the scale test–retest reliability at 6 months because that was the time criterion selected by Nock et al.1 in the validation of the original scale.
Data analysisInstead of examining a single construct using numerous items (as the BSS10 does, for example), the SITBI was designed to efficiently examine a wide range of constructs utilising a minimum number of items. Consequently, following the practice of Nock et al.,1 factorial and internal consistency analyses were omitted, as they would have no theoretical or empirical relevance. In their place, we first examined the descriptive statistics (mean, standard deviation [SD] or proportion of each quantitative EPCA item) and then the inter-rater reliability for each quantitative item (there were 5 raters in this study). To do so, we used the kappa statistic, which examines to what degree 2 independent raters coincide when scoring a specific item from various randomly selected interviews (n=15). The kappa coefficient takes values from −1 to 1. A value of k=0 reflects that the concordance observed is exclusively due to chance. Values above 0.75 correspond to excellent inter-rater agreement; values between 0.40 and 0.75 correspond to good agreement and values less than 0.40 reflect poor inter-rater agreement.16
We then examined the test–retest reliability of the items referring to the presence of frequence of each suicidal behaviour (n=50). To do so, we examined the correspondence between items assessing the presence of a suicidal behaviour (Items 1, 30, 58, 84, 116 and 143, which assess the presence/absence of suicidal ideation, suicide plans, suicidal gestures, suicide attempts, self-injuries and self-injurious thoughts, respectively) at the moment of the first interview and in the follow-up interview. To check test–retest reliability of the items referring to the frequency of the different types of suicidal behaviour, we used the intraclass correlation coefficient (ICC).17
Lastly, we examined the construct validity of the scale, checking the correspondence between the EPCA and other related scales (described in the previous section). In addition to the reliability of the EPCA as an assessment instrument, it was important to show that it is a valid measure of the constructs of suicidal behaviour.18 We examined the validity of the scale testing the consistence of the answers to the items related to presence of suicidal ideation (Item 1), suicide plans (Item 30) and suicidal attempts (Item 84) with the answers to the similar items on BSS scale10 (specifically, Blocks II, III and IV, respectively). We also checked the consistency of the answers related to the presence of suicidal gestures on the EPCA (Item 58) with the answers to Item 9 on the BSS (related to the purpose of the attempt) and we compared the frequency of suicide attempts according to the EPCA (Item 88 with the response to Item 18 on the BSS). Likewise, we compared the consistency of the answers to some characteristics of the suicide attempts, such as: having consumed alcohol or drugs in the moment of the attempt (Item 110 on the EPCA and Item 19 on the SIS11), degree of premeditation (Item 97 on the EPCA and Item 15 on the SIS) and method used (Item 92 on the EPCA and answers to the LRS12 and Item 1 on the RRS13).
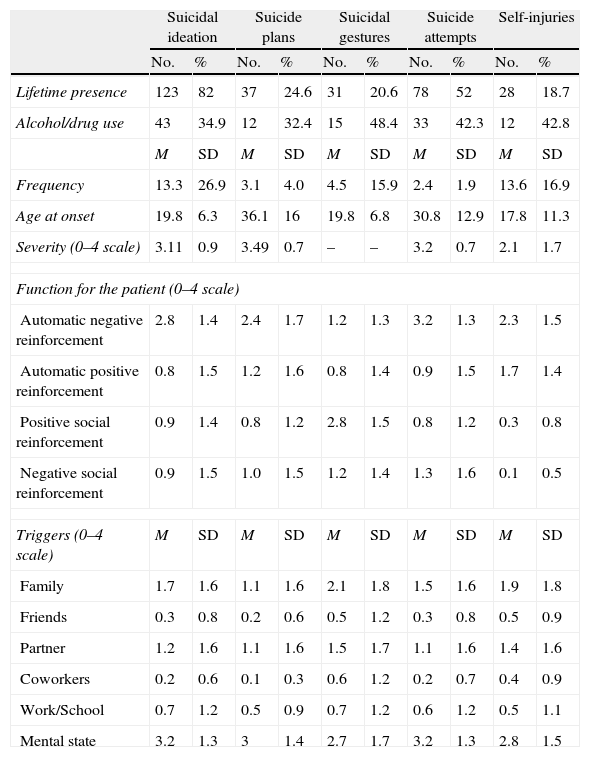
ResultsDescriptive statisticsThe frequencies, means and standard deviations of the participants’ answers are shown in Table 2. As this table indicates, given that this was a sample of hospitalised patients (and in many cases after a suicide attempt), the rate of each type of self-injurious behaviour was high, especially in the case of suicidal ideation and suicide attempts. The high rate of consumption of alcohol/drugs at the moment of carrying out self-injurious behaviour was also notable (with a rate of 48.4% in the case of suicidal gestures).
Frequencies, means (M) and standard deviations (SD) for the participants’ answers on the EPCA scale.
| Suicidal ideation | Suicide plans | Suicidal gestures | Suicide attempts | Self-injuries | ||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | |
| Lifetime presence | 123 | 82 | 37 | 24.6 | 31 | 20.6 | 78 | 52 | 28 | 18.7 |
| Alcohol/drug use | 43 | 34.9 | 12 | 32.4 | 15 | 48.4 | 33 | 42.3 | 12 | 42.8 |
| M | SD | M | SD | M | SD | M | SD | M | SD | |
| Frequency | 13.3 | 26.9 | 3.1 | 4.0 | 4.5 | 15.9 | 2.4 | 1.9 | 13.6 | 16.9 |
| Age at onset | 19.8 | 6.3 | 36.1 | 16 | 19.8 | 6.8 | 30.8 | 12.9 | 17.8 | 11.3 |
| Severity (0–4 scale) | 3.11 | 0.9 | 3.49 | 0.7 | – | – | 3.2 | 0.7 | 2.1 | 1.7 |
| Function for the patient (0–4 scale) | ||||||||||
| Automatic negative reinforcement | 2.8 | 1.4 | 2.4 | 1.7 | 1.2 | 1.3 | 3.2 | 1.3 | 2.3 | 1.5 |
| Automatic positive reinforcement | 0.8 | 1.5 | 1.2 | 1.6 | 0.8 | 1.4 | 0.9 | 1.5 | 1.7 | 1.4 |
| Positive social reinforcement | 0.9 | 1.4 | 0.8 | 1.2 | 2.8 | 1.5 | 0.8 | 1.2 | 0.3 | 0.8 |
| Negative social reinforcement | 0.9 | 1.5 | 1.0 | 1.5 | 1.2 | 1.4 | 1.3 | 1.6 | 0.1 | 0.5 |
| Triggers (0–4 scale) | M | SD | M | SD | M | SD | M | SD | M | SD |
| Family | 1.7 | 1.6 | 1.1 | 1.6 | 2.1 | 1.8 | 1.5 | 1.6 | 1.9 | 1.8 |
| Friends | 0.3 | 0.8 | 0.2 | 0.6 | 0.5 | 1.2 | 0.3 | 0.8 | 0.5 | 0.9 |
| Partner | 1.2 | 1.6 | 1.1 | 1.6 | 1.5 | 1.7 | 1.1 | 1.6 | 1.4 | 1.6 |
| Coworkers | 0.2 | 0.6 | 0.1 | 0.3 | 0.6 | 1.2 | 0.2 | 0.7 | 0.4 | 0.9 |
| Work/School | 0.7 | 1.2 | 0.5 | 0.9 | 0.7 | 1.2 | 0.6 | 1.2 | 0.5 | 1.1 |
| Mental state | 3.2 | 1.3 | 3 | 1.4 | 2.7 | 1.7 | 3.2 | 1.3 | 2.8 | 1.5 |
Automatic negative reinforcement: to get rid of negative feelings; automatic positive reinforcement: to feel something, because you feel numb or empty; negative social reinforcement: to avoid doing something or escape from something or someone; positive social reinforcement: to communicate with another person or manage to attract their attention.
As for the frequency of each behaviour type, the one that occurred with greatest lifetime frequency was suicidal ideation. In contrast, the type that occurred least often was suicide attempts. With respect to onset, the behaviours that happened at the earliest ages were the self-injuries. Suicide plans, on the contrary, were initiated around 36 years of age.
The most important function that suicidal ideation, suicide plans, suicide attempts and self-injuries fulfilled for the patients was automatic negative reinforcement (that is, that patients usually present self-injurious ideation, plan their suicides, attempt to commit suicide and/or injure themselves to escape from other negative feelings). However, it is noteworthy that the most important function that suicidal gestures fulfilled for the patients was positive social reinforcement (to get the attention of a person or communicate with someone).
With respect to triggers, the factor that contributed most to the performance of self-injurious behaviour was the patient's mental state at the moment of carrying out the action. Family and partner problems followed as the next most frequent contributors. This finding is similar to that found by Nock et al.1
As for suicide attempts (n=121), the most frequently used methods were overdose of medicines (70.5%), illegal drugs (16.6%) and deep cuts (14.1%). Other suicide methods such as firearms (10.2%), immolation (8.9%) or hanging (8.9%) were less frequent in our setting. Financial problems constituted the triggering factor for the most recent suicide attempt in 33.3% of the attempts, followed by arguments with the partner (25.6%) and family arguments (17.9%). Impulsive, non-premeditated suicide attempts constituted 67.9%, and they were decided on the same day in which the attempt occurred. Finally, the participants had carried out a mean of 1.4 previous suicide attempts (SD=1.96).
Psychometric propertiesInter-rater reliabilityOur analysis revealed perfect agreement among examiners (k=1) for all the items that assessed the presence of lifetime suicidal behaviour (Items 1, 30, 58, 84, 116 and 143, which assessed the presence/absence of suicidal ideation, suicide plans, suicidal gestures, suicide attempts, self-injurious thoughts and self-injuries, respectively). Inter-rater reliability was also perfect (k=1) for all items assessing the presence of a suicidal behaviour in the previous year (Items 5, 34, 62, 89 and 147) and in the previous month (Items 6, 35, 63, 90 and 148). For the rest of quantitative items (age, number of episodes), the reliability coefficient obtained was excellent (k=0.90). Inter-rater reliability was not calculated for qualitative items (e.g., open questions on the reasons for performing self-injurious behaviours), given the nature of the data.
Test–retest reliabilityThe test–retest reliability was very good for suicidal ideation (Item 1, k=0.82), suicide plans (Item 30, k=0.79) and suicide attempts (Item 84, k=0.87). However, this reliability was less in the case of self-injuries (Item 143, k=0.65) and suicidal gestures (Item 58, k=0.47).
Test–retest reliability was very good in the case of frequency of suicidal ideation (Item 4, ICC=0.77), suicide plans (Item 33, ICC=0.69) and suicide attempts (Item 88, ICC=0.91). However, test–retest reliability was lower for suicidal gestures (Item 61, ICC=38) and self-injuries (Item 146, ICC=0.49).
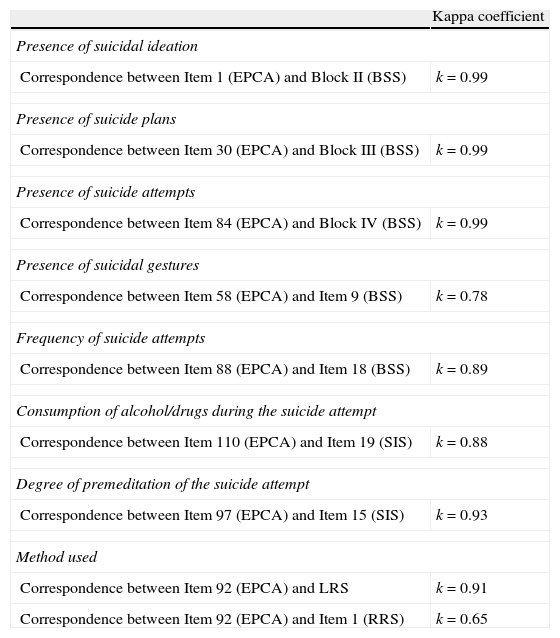
Construct validityThe results related to construct validity are shown in Table 3. In general, agreement among the answers was very good, ranging between k=0.65 in the case of the method used (comparing it with Item 1 on the RRS13) and k=0.99 for the presence of suicidal ideation, suicide plans and suicide attempts.
Construct validity.
| Kappa coefficient | |
| Presence of suicidal ideation | |
| Correspondence between Item 1 (EPCA) and Block II (BSS) | k=0.99 |
| Presence of suicide plans | |
| Correspondence between Item 30 (EPCA) and Block III (BSS) | k=0.99 |
| Presence of suicide attempts | |
| Correspondence between Item 84 (EPCA) and Block IV (BSS) | k=0.99 |
| Presence of suicidal gestures | |
| Correspondence between Item 58 (EPCA) and Item 9 (BSS) | k=0.78 |
| Frequency of suicide attempts | |
| Correspondence between Item 88 (EPCA) and Item 18 (BSS) | k=0.89 |
| Consumption of alcohol/drugs during the suicide attempt | |
| Correspondence between Item 110 (EPCA) and Item 19 (SIS) | k=0.88 |
| Degree of premeditation of the suicide attempt | |
| Correspondence between Item 97 (EPCA) and Item 15 (SIS) | k=0.93 |
| Method used | |
| Correspondence between Item 92 (EPCA) and LRS | k=0.91 |
| Correspondence between Item 92 (EPCA) and Item 1 (RRS) | k=0.65 |
BSS: Beck scale of suicide ideation; EPCA: Self-Injurious Thoughts and Behaviors Interview; LRS: lethality rating scale; RRS: risk-rescue scale; SIS: suicide intent scale.
The concordance with respect to suicidal gestures was slightly lower than that obtained for the rest of suicidal behaviours (k=0.78). The concordance obtained for the method used (k=0.65) was also lower.
DiscussionOur results back the reliability (both inter-rater and test–retest) and validity of the EPCA in the Spanish population. Although there are many measures that examine specific suicidal behaviours (such as the BSS10), there are no other scales in our country that assess the entire range of suicidal behaviour (suicidal ideation, suicide plans, suicidal gestures, suicide attempts and self-injurious behaviours). Likewise, in Spain there are no scales that differentiate between suicidal gestures and suicide attempts. This distinction is vitally important because, compared with the individuals that carry out suicidal gestures, the ones that try to commit suicide with the intention of dying have a greater risk of dying in a later suicide attempt19–21 or of carrying out a more lethal suicide attempt.22,23 In addition, the EPCA extends the existing scales greatly, as it also contains items that collect information on the subject's motivation for having carried out suicidal behaviour and on the triggering events. For all these reasons, we consider the EPCA useful for assessing the suicidal risk of a given patient, one of the most important, and the most complex, tasks in clinical practice.24
As for the psychometric properties of the EPCA, the excellent inter-rater reliability observed for each type of suicidal behaviour examined seems to be related to the clarity and precision with which each type is defined. Our analyses also revealed that test–retest reliability was between good and excellent in all the suicidal behaviours examined. In general, we can conclude the coefficients of test–retest reliability indicate that the data obtained with the EPCA are stable. The reliability obtained was greater than that obtained using other instruments.25,26 The lower reliability obtained for suicidal gestures may be related to the limited number of patients that indicated in the follow-up interview that they had ever made a suicidal gesture. Specifically, of the 31 patients that stated in the first interview that they had made a suicidal gesture, only 13 made the same statement in the follow-up interview. The reason why some patients changed their answer to this item is unclear. A suicidal gesture can be interpreted as an attempt to manipulate and mobilise the people in the surroundings, and some people are not always willing to admit that those are their intentions.
Likewise, our results support the fact that the answers obtained using our scale are consistent with those of other measures of suicidal behaviour (the BSS,10 SIS,11 LRS12 and RRS13), thus backing the construct validity of our scale. However, the fact that the concordance with respect to suicidal gestures was slightly lower than that obtained for the rest of the suicidal behaviours may be related to the definition itself of the suicidal gesture. In the EPCA scale, it is defined as any behaviour carried out by a person so that others believe that the person had the intention of killing themself when in fact this intention did not really exist. Item 9 on the BSS,10 in contrast, refers to a more precise motivation (to manipulate the surroundings, to attract attention or for revenge), not to simply making the others believe that the person wanted to kill themself. The lower concordance found in this case is probably related to the fact that the 2 items are worded differently. The concordance obtained for method used (k=0.65) was also lower. In this case, this is due to the different way of grouping the methods: in the SITBI scale, there are up to 15 different methods; in contrast, the RRS13 classifies all the methods into 3 blocks: (a) ingestion, cutting, stabbing; (b) drowning, suffocation, strangling; and (c) jumping, shooting.
Although the objective of this study did not include analysing the sample characteristics, some of the findings deserve at least a comment. The high rate of consumption of intoxicants in the entire range of suicidal behaviours is worth pointing out. In this sense, some authors have found a strong association between suicidal behaviour and substance abuse, especially in the case of cocaine consumers.27,28 Another significant finding is the fact that self-injuries commence at an earlier age than suicide plans. This might be due to the fact that such behaviours fulfil different functions for the subjects. Self-injuries could have a stress-releasing function,29 while planning might be more closely related to depressive processes or loneliness.30 As for triggers and methods used, our findings are similar to what the literature reflects.31
In summary, we can conclude that the EPCA possesses good psychometric properties. However, for interpreting these results, it is important to bear in mind some limitations. As this is a pilot study, the scale was validated in a relatively small patient sample (n=150); consequently, the data presented here should be considered preliminary. The participants in this study were seen in the emergency and the hospitalisation services of the Fundación Jiménez Díaz. Consequently, administering the EPCA in other settings (e.g., outpatient services) is needed to test the generalisability of these results. In addition, although our scale examines a wide range of suicidal behaviours, its scope is limited. For example, it does not include items on potentially self-destructive behaviours, such as alcohol consumption or substance abuse. Neither does it assess psychological states frequently associated with suicidal behaviour, such as depressive mood or despair. Understanding the influence that other self-destructive behaviours and these psychological states have on suicidal behaviour is essential to understanding suicidal behaviour. It might therefore be useful to add additional modules that collect this type of information. Likewise, no cultural adaptation of the scale was performed, which could limit its usefulness with Spanish-speakers residing outside of Spain (e.g., Hispanics in the USA).
Finally, it is worth emphasising that, given that the estimated time it takes to administer the scale ranges between 3 and 15min, applying it in the daily clinical practice in our setting is viable. The screening questions that head each module take less than 3min; the benefits, in contrast, are many: administering the scale can have a legal implication and serve as a basis for clinical decisions.32 In addition, if the screening is positive, administering the scale can help to improve the format in which the information is collected and help to make clinical evaluation more complete.33 For these reasons, we consider that the EPCA scale can be useful in our clinical practice.
Ethical disclosuresProtection of human and animal subjectsThe authors state that no experiments were carried out on human being or animals for this research.
Confidentiality of dataThe authors state that they followed their work centre protocols on publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in this study.
Right to privacy and informed consentThe authors state that no patient data appears in this article.
Conflict of interestThe authors have no conflicts of interests to declare.
This article was made possible thanks to the research project «Assessment of self-injurious behaviours and suicidal gestures: validation of the Self-Injurious Thoughts and Behaviours Interview (SITBI)» (2011) funded by the Bank of Mental Health Instruments (BICIBERSAM in Spanish) and to the Río Hortega research training fellowship for health professionals that have finished their specialised health training (CM10/00034). Likewise, the authors wish to express their appreciation to Dr Matthew Nock for permission to translate and validate the SITBI.
Please cite this article as: García-Nieto R, et al. Traducción y validación de la Self-Injurious Thoughts and Behaviours Interview en población española con conducta suicida. Rev Psiquiatr Salud Ment (Barc.).2013;6:101–8.