Abstract
Background
There are increasing data on the potential risk of pancreatic carcinoma associated with glucagon-like peptide 1 receptor agonists (GLP-1RAs).
Aim
The study aimed to determine whether GLP-1RAs are associated with increased detection of pancreatic carcinoma based on the FDA Adverse Events Reporting System and clarify its potential mechanisms through keyword co-occurrence analysis from literature database.
Method
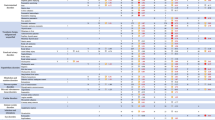
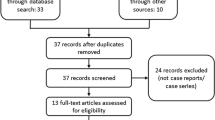
Disproportionality and Bayesian analyses were used for signal detection using reporting odds ratio (ROR), proportional reporting ratio (PRR), information component (IC), and empirical Bayesian geometric mean (EBGM). Mortality, life-threatening events, and hospitalizations were also investigated. VOSviewer was adopted to generate visual analysis of keyword hotspots.
Results
A total of 3073 pancreatic carcinoma cases were related to GLP-1RAs. Five GLP-1RAs were detected with signals for pancreatic carcinoma. Liraglutide had the strongest signal detection (ROR 54.45, 95% CI 51.21–57.90; PRR 52.52, 95% CI 49.49–55.73; IC 5.59; EBGM 48.30). The signals of exenatide (ROR 37.32, 95% CI 35.47–39.28; PRR 36.45, 95% CI 34.67–38.32; IC 5.00; EBGM 32.10) and lixisenatide (ROR 37.07, 95% CI 9.09–151.09; PRR 36.09; 95% CI 9.20–141.64; IC 5.17, EBGM 36.09) were stronger than those of semaglutide (ROR 7.43, 95% CI 5.22–10.57; PRR 7.39; 95% CI 5.20–10.50; IC 2.88, EBGM 7.38) and dulaglutide (ROR 6.47, 95% CI 5.56–7.54; PRR 6.45; 95% CI 5.54–7.51; IC 2.67, EBGM 6.38). The highest mortality rate occurred in exenatide (63.6%). Based on the bibliometric investigation, cAMP/protein-kinase, Ca2+ channel, endoplasmic-reticulum stress, and oxidative stress are potential pathogenesis of pancreatic carcinoma resulting from GLP-1RAs.
Conclusion
Based on this pharmacovigilance study, GLP-1RAs, except albiglutide, are associated with pancreatic carcinoma.



Similar content being viewed by others
References
Meier JJ. GLP-1 receptor agonists for individualized treatment of type 2 diabetes mellitus. Nat Rev Endocrinol. 2012;8(12):728–42.
Tian L, Jin T. The incretin hormone GLP-1 and mechanisms underlying its secretion. J Diabetes. 2016;8(6):753–65.
Drucker DJ. Mechanisms of action and therapeutic application of glucagon-like peptide-1. Cell Metab. 2018;27(4):740–56.
Holst JJ. From the incretin concept and the discovery of GLP-1 to today’s diabetes therapy. Front Endocrinol. 2019;10:260.
Deacon CF, Nauck MA, Toft-Nielsen M, et al. Both subcutaneously and intravenously administered glucagon-like peptide I are rapidly degraded from the NH2-terminus in type II diabetic patients and in healthy subjects. Diabetes. 1995;44(9):1126–31.
Aroda VR. A review of GLP-1 receptor agonists: evolution and advancement, through the lens of randomised controlled trials. Diabetes Obes Metab. 2018;20(Suppl 1):22–33.
Derosa G, Maffioli P. GLP-1 agonists exenatide and liraglutide: a review about their safety and efficacy. Curr Clin Pharmacol. 2012;7(3):214–28.
Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–701.
de Heer J, Goke B. Are incretin mimetics and enhancers linked to pancreatitis and malignant transformations in pancreas? Expert Opin Drug Saf. 2014;13(11):1469–81.
Gale EA. GLP-1 based agents and acute pancreatitis: drug safety falls victim to the three monkey paradigm. BMJ. 2013;346: f1263.
Denker PS, Dimarco PE. Exenatide (exendin-4)-induced pancreatitis: a case report. Diabetes Care. 2006;29(2):471.
Bain SC, Stephens JW. Exenatide and pancreatitis: an update. Expert Opin Drug Saf. 2008;7(6):643–4.
Mali G, Ahuja V, Dubey K. Glucagon-like peptide-1 analogues and thyroid cancer: an analysis of cases reported in the European pharmacovigilance database. J Clin Pharm Ther. 2021;46(1):99–105.
Santella C, Yin H, Hicks BM, et al. Weight-lowering effects of glucagon-like peptide-1 receptor agonists and detection of breast cancer among obese women with diabetes. Epidemiology. 2020;31(4):559–66.
Elashoff M, Matveyenko AV, Gier B, et al. Pancreatitis, pancreatic, and thyroid cancer with glucagon-like peptide-1-based therapies. Gastroenterology. 2011;141(1):150–6.
Butler PC, Elashoff M, Elashoff R, et al. A critical analysis of the clinical use of incretin-based therapies: are the GLP-1 therapies safe? Diabetes Care. 2013;36(7):2118–25.
Cure P, Pileggi A, Alejandro R. Exenatide and rare adverse events. N Engl J Med. 2008;358:1969–72.
Butler AE, Campbell-Thompson M, Gurlo T, et al. Marked expansion of exocrine and endocrine pancreas with incretin therapy in humans with increased exocrine pancreas dysplasia and the potential for glucagon-producing neuroendocrine tumors. Diabetes. 2013;62(7):2595–604.
Spranger J, Gundert-Remy U, Stammschulte T. GLP-1-based therapies: the dilemma of uncertainty. Gastroenterology. 2011;141(1):20–3.
Matveyenko AV, Dry S, Cox HI, et al. Beneficial endocrine but adverse exocrine effects of sitagliptin in the human islet amyloid polypeptide transgenic rat model of type 2 diabetes: interactions with metformin. Diabetes. 2009;58(7):1604–15.
Wu S, Wang J, Jing L, et al. A diabetic patient complicated with pancreatic cancer after using liraglutide: a case report. Front Endocrinol. 2020;11:608966.
Azoulay L, Filion KB, Platt RW, et al. Incretin based drugs and the risk of pancreatic cancer: international multicentre cohort study. BMJ. 2016;352: i581.
Knapen LM, van Dalem J, Keulemans YC, et al. Use of incretin agents and risk of pancreatic cancer: a population-based cohort study. Diabetes Obes Metab. 2016;18(3):258–65.
Monami M, Nreu B, Zannoni S, et al. Effects of SGLT-2 inhibitors on diabetic ketoacidosis: a meta-analysis of randomised controlled trials. Diabetes Res Clin Pract. 2017;130:53–60.
Pinto LC, Falcetta MR, Rados DV, et al. Glucagon-like peptide-1 receptor agonists and pancreatic cancer: a meta-analysis with trial sequential analysis. Sci Rep. 2019;9(1):2375.
Cao C, Yang S, Zhou Z. GLP-1 receptor agonists and risk of cancer in type 2 diabetes: an updated meta-analysis of randomized controlled trials. Endocrine. 2019;66(2):157–65.
Zhang X, Wang M, Wang X, et al. Comparison of New glucose-lowering drugs on the risk of pancreatitis in type 2 diabetes: a network meta-analysis. Endocr Pract. 2022;28(3):333–41.
Egan AG, Blind E, Dunder K, et al. Pancreatic safety of incretin-based drugs–FDA and EMA assessment. N Engl J Med. 2014;370(9):794–7.
Cao M, Wang L, Zhang L, et al. Global publication trends and hotspots of molecular biomarkers in DILI from 1991 to 2020: a 30-year bibliometric analysis. Sci Prog. 2021;104(1):311971031.
Holst JJ, Orskov C, Nielsen OV, et al. Truncated glucagon-like peptide I, an insulin-releasing hormone from the distal gut. FEBS Lett. 1987;211(2):169–74.
Brown E, Wilding J, Barber TM, et al. Weight loss variability with SGLT2 inhibitors and GLP-1 receptor agonists in type 2 diabetes mellitus and obesity: mechanistic possibilities. Obes Rev. 2019;20(6):816–28.
Sarafidis P, Ferro CJ, Morales E, et al. SGLT-2 inhibitors and GLP-1 receptor agonists for nephroprotection and cardioprotection in patients with diabetes mellitus and chronic kidney disease. A consensus statement by the EURECA-m and the DIABESITY working groups of the ERA-EDTA. Nephrol Dial Transplant. 2019;34(2):208–30.
Palmer SC, Tendal B, Mustafa RA, et al. Sodium-glucose cotransporter protein-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. BMJ. 2021;372: m4573.
Sakaeda T, Tamon A, Kadoyama K, et al. Data mining of the public version of the FDA Adverse Event Reporting System. Int J Med Sci. 2013;10(7):796–803.
Lewis AL, Mcentee N, Holland J, et al. Development and approval of rybelsus (oral semaglutide): ushering in a new era in peptide delivery. Drug Deliv Transl Res. 2022;12(1):1–6.
Aaseth J, Ellefsen S, Alehagen U, et al. Diets and drugs for weight loss and health in obesity—an update. Biomed Pharmacother. 2021;140: 111789.
Wang L, Feng W, Duan J, et al. Pharmacovigilance bibliometrics: visualizing thematic development in the category of pharmacology and pharmacy in web of science. Front Pharmacol. 2021;12: 731757.
Michel C, Scosyrev E, Petrin M, et al. Can disproportionality analysis of post-marketing case reports be used for comparison of drug safety profiles? Clin Drug Investig. 2017;37(5):415–22.
Raschi E, Poluzzi E, Salvo F, et al. Pharmacovigilance of sodium-glucose co-transporter-2 inhibitors: what a clinician should know on disproportionality analysis of spontaneous reporting systems. Nutr Metab Cardiovasc Dis. 2018;28(6):533–42.
Acknowledgements
None.
Funding
This study was supported by the Chinese Society of Toxicology Clinical Toxicology Project (number CST2020CT109) and the Beijing Hospital Authority Youth Programme (number QML20180503).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The placement of graph in Table 3 is corrected.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cao, M., Pan, C., Tian, Y. et al. Glucagon-like peptide 1 receptor agonists and the potential risk of pancreatic carcinoma: a pharmacovigilance study using the FDA Adverse Event Reporting System and literature visualization analysis. Int J Clin Pharm 45, 689–697 (2023). https://doi.org/10.1007/s11096-023-01556-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-023-01556-2